Impact of Drug Abuse on Youth: A Growing Concern
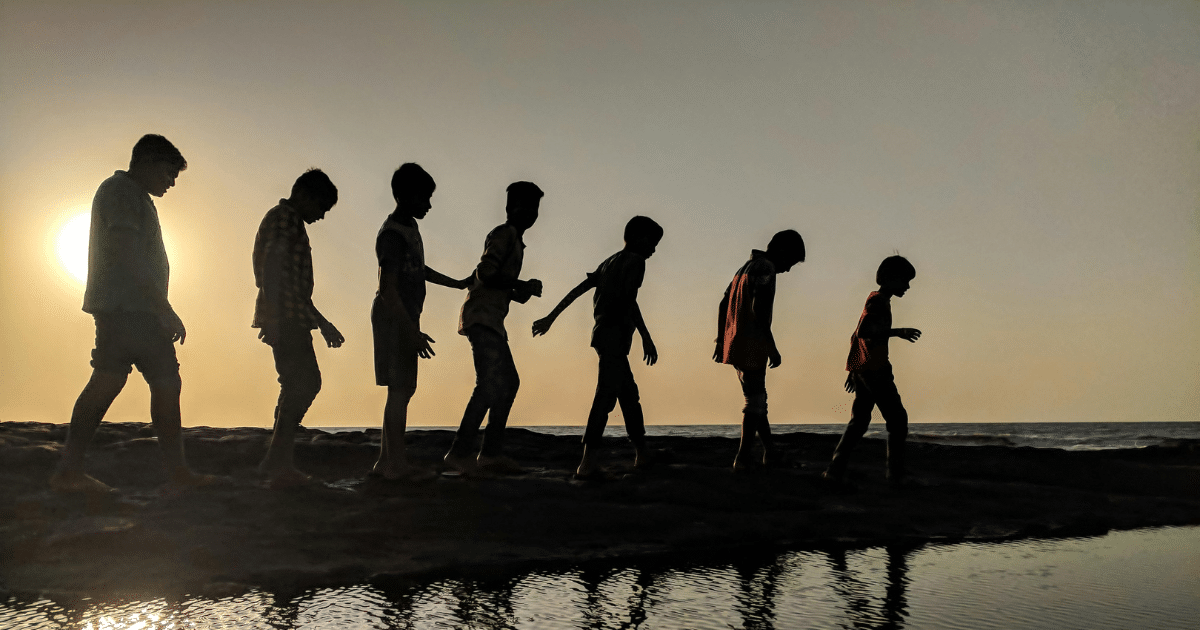
From high school parties to social media trends, the influence of today’s youth is bathed in more drug-related influences than ever before, and the results are straight out of the Twilight Zone. Drug abuse problems amongst the youth aren’t just one-off incidents; They are a nationwide crisis concerning families, schools, and communities. The National Center for Drug Abuse Statistics found that more than 46 percent of teens have used illicit drugs before completing high school, with rates over 11 percent among 12 to 17-year-olds misusing prescription medications. These figures aren’t figures, they’re warning lights flashing across an entire generation.
The prime reason why teen substance use is particularly dangerous is that the age at which it interferes with is particularly crucial. Adolescence is a time of identity formation, emotional development, and academic growth, but drugs can short-circuit all of this.
From underage drinking at the weekend party to potential vaping habits during a class break, these habits can quickly turn into adolescent addiction without anyone really noticing a problem. And since young brains are still under development, drug use in the long run may be more harmful than in adults. That’s the reason early intervention programs, youth drug prevention efforts, as well as young adult rehabilitation resources, are going to be even more crucial now than ever.
The Reality of Drug Abuse Among Youth
Teenage years are often characterized by fun and discovery on the part of the young, but this isn’t the case for many teens because there is a problem with drug abuse among youth. Today’s teenagers are entering a complicated world where access to substances is less difficult, peer pressure has a greater effect via social media, and mental illness is increasing.

Many teens play with drugs out of curiosity, to fit in, or as a coping mechanism for anxiety, depression, and trauma. However, younger minds are more susceptible, so they are more likely to be addicted. To understand where we are in terms of trends and the most commonly misused substances, we can create better informed youth drug prevention strategies based on what prevents kids from using specific substances.
Trends in Teen Substance Use
Teen substance use is not a fixed problem; it adjusts to cultural trends, access, and public view. In the U.S., trends in youth drug use over the last years are shown below:
| Substance | Trend | Notable Stats |
| Vaping (nicotine & THC) | Rising use among middle and high schoolers | 14.1% of high schoolers vaped in the past month |
| Cannabis | Growing normalization | Over 22% of 12th graders used marijuana in the past year |
| Alcohol | Slight decline, but still high | 29% of teens report underage drinking in 30 days |
| Prescription drugs | Misuse remains a concern | 5.5% of teens misused prescription painkillers in 2024 |
Commonly Abused Substances in Adolescents
Things come and go in the realm of trends, but several substances stay consistent with reports of teenage substance misuse. These drugs are usually selected because of the availability and popularity of the class, but their effects can cause a change in the person’s life.
| Substance | Why Teens Use It | Risks Involved |
| Alcohol | Peer pressure, party culture | Liver damage, poor decision-making, and risk of dependency |
| Marijuana | Relaxation, social bonding | Cognitive impairment, motivation loss, and long-term addiction |
| Nicotine (vapes) | Flavors, stress relief, peer influence | Lung issues, nicotine addiction, a gateway to other substances |
| Prescription meds | Academic pressure, self-medication | Overdose, dependency, severe withdrawal symptoms |
| Hallucinogens | Curiosity, peer experimentation | Mental health disturbances, unsafe behavior |
Signs and Symptoms of Drug Abuse in Young People
Early identification of the warning signs of teenage substance misuse could mean the difference between receiving an intervention before addiction sets in. Because teens try anything to cover their behavior, parents, teachers, and peers need to be on the lookout for the slightest physical, emotional, and behavioral signs. Even though not all signs indicate a young person is taking drugs, some pattern of these behaviors may indicate a much bigger problem.
Here are common indicators of drug abuse problems in youth:
- Impulse tendencies, unpredictable outbursts, or an unexpected change of mood
- Loss of interest in various hobbies, school, or social activities.
- Poor performance at school or continuous absences from school.
- Lack of hygiene or radical physical appearance changes.
- Secret or even isolating from family and old friends.
- Unusual sleeping or eating patterns
- Red eyes, nosebleed, or continuing cough
- Visiting any drug paraphernalia, such as rolling papers, vape pens, and pill bottles.
- Regularly requesting money or things disappearing at home
- Behaving recklessly or taking a risk, but without considering the consequences
Causes and Risk Factors for Drug Abuse in Adolescents
Drug abuse issues among youth don’t have a single cause – it is a result of the combined effect of the personal, social, and environmental circumstances. Below you will find some of the most common causes and risk factors that contribute to teen substance abuse and adolescent addiction:
Causes:
- Emotional and mental health struggles (e.g., anxiety, depression, trauma)
- Peer pressure and social influence from friends or social media
- Lack of parental supervision or unstable family dynamics
Risk Factors:
- Genetic predisposition or family history of substance abuse
- Low self-esteem, poor coping skills, or unresolved emotional issues
- Exposure to drugs in the community or limited access to youth drug prevention programs
The Role of Family and Community in Preventing Drug Abuse
Maintaining drug abuse problems among youth needs more than programs that target them in schools or scare tactics, but it also needs the environment that surrounds teens. Family dynamics also play a large societal role in determining the attitudes of a young person toward substance use. A caring home and neighborhood can offer the direction, responsibility, and nurturing that will help adolescents avoid risky behaviors.
Parents are privileged to practice healthy behaviors and talk about the risks of teen substance use in an open manner. Guardians and mentors are also provided with their unique chance to practice healthy behaviors and communicate openly about the threats of teen substance use. At the same time, communities that provide positive activities, youth engagement programs, and easy access to mental health resources are more likely to create resilience and help reduce the rates of adolescents being addicted.
Building a Supportive Home Environment
| Strategy | How It Helps Prevent Drug Use |
| Open and honest communication | Builds trust and allows teens to express concerns before turning to substances |
| Setting clear rules and expectations | Helps teens understand boundaries and the consequences of teenage substance misuse |
| Parental involvement in a teen’s life | Increases emotional support and reduces opportunities for risky behavior |
| Modeling healthy coping behaviors | Shows teens how to handle stress without turning to drugs or underage drinking |
| Encouraging responsibility and goals | Builds self-worth and reduces vulnerability to peer pressure |
Effective Strategies for Addressing Drug Abuse in Youth
The challenge of handling the issue of drug abuse amongst youth calls for a multi-tiered approach involving the work of schools, families, healthcare providers, and community leaders. It is not enough just to discourage teens from using substances. They should also learn useful information, find new resources, and discover better ways to spend their time. Scientifically tested prevention programs, regular teenage addicts’ danger awareness, and the care of adolescents’ mental health are the most important weapons in the struggle against teenage addiction.
Early intervention programs must help to detect youth at risk before substance use increases. School counselors, pediatricians, and youth mentors can play the role of frontline defenders by being aware of warning signs and making appropriate referrals to young adult rehabilitation services. In addition, the development of life values such as stress abatement, decision making, and resisting peer pressure will also greatly reduce the allure of drugs. A strong defense against teenage substance misuse is built with supportive family relationships and youth proactive drug prevention policies on the side of these strategies.
Importance of Early Intervention and Support Systems
Early intervention is the survivor’s key between experimentation and permanent adolescent addiction. When such warning signs of teenage substance misuse are attended to early, compassionately, and with evidence-based strategies, teens stand a much better chance at regaining their health and a healthy future. Research reveals that early intervention by a youth can prevent chronic substance use disorders when he/she is an adult.
Support systems in this process play a key role in it. Healthier nutrition choices by young people depend on confident adults leading, teaching, and encouraging them in schools. When these systems help teens manage anxiety, withstand peer pressure, or even come back through young adult reeducation, they can literally be lifesavers.
Get Help Today with Silicon Valley Recovery
If you or someone you care about is struggling with drug abuse issues in their youth, don’t wait for things to get worse. At Silicon Valley Recovery, we excel in compassionate, personalized, and young adult services for teen substance use, adolescent addiction, and underage drinking. We provide individualized treatment plans, care for the family, and evidence-based therapies for long-term recovery.
FAQs
How does peer influence impact substance misuse prevention in adolescents?
Peer influence that leaned to the positive side would encourage positive behavior and resistance to teen substance use. On the other hand, negative social circles act as a conduit through which the probability of adolescent addiction increases via the normalization of the use of drugs and alcohol.
What role does family support play in addiction awareness and mental health intervention for youth?
Robust family relation provides emotional security and help detect behavioral changes. This sort of support is essential for successful mental health intervention and substance misuse aggravation prevention.
What are the benefits of education programs in preventing drug abuse problems in youth?
Youth drug prevention efforts provide teens with awareness of the possible consequences of drugs and also teach teens skills for making good decisions. Such programs have been proven to decrease teenage substance abuse and defer the use of drugs for the first time.
How can counseling services aid in adolescent rehabilitation for substance misuse issues?
Counseling provides an environment for teens to discuss the underlying emotional problems, trauma, or peer pressure. It also refers them to coping strategies and young adult rehabilitation resources.
What are the key components of effective mental health intervention strategies for youth dealing with addiction?
Effective strategies include:
- Early detection
- Family involvement
- Personalized treatment
- Access to ongoing mental health and recovery services